SKIN TUMORS AND LESIONS
The skin is the largest organ of the human body and one of its main functions is to protect muscles, cartilage, bones, and other tissues. During the various stages of life, factors such as genetic predisposition and prolonged sun exposure can give rise to skin tumors, skin neoplasms or dermatological neoplasms, which are abnormal growths of skin cells that can be benign (harmless), premalignant (can become malignant) or malignant (skin cancer).
As a country with a tropical climate, Brazil receives a great incidence of sunlight. Statistical data reveal that about 75% of the solar radiation received throughout life occurs in the first 20 years and 90% of tumors and lesions develop on the parts of the body that are exposed to the sun, usually after the age of 40. According to INCA (National Cancer Institute), the number of Skin Tumors and Lesions has been increasing in recent years. This is due in large part to a combination of improved diagnoses, people getting more exposure to the sun, and people living longer.
WHAT IT IS AND HOW IT IS DONE
Plastic surgery is used to remove Skin Tumors and Lesions, as it uses specialized techniques to preserve the health and appearance of the skin. Excision, curettage, electrodissection, among others, are effective in most procedures. In highly complex cases, we can use flaps (tissues from neighboring areas with the same arterial nutrition) or grafts (from the distant site).
When the surgical procedure is indicated – or more than one of them – we look for the best planning taking into consideration the possible aesthetic and functional result for each patient. If necessary, we refer the patient to other specialized professionals to complement the treatment.
Removal of benign and malignant tumors can be done through the following treatments:
Skin Biopsy – A procedure in which a small fragment of the skin or mucous membrane is removed for pathological analysis. It can be done with a punch (a cylinder with a cutting surface that when rotated goes deeper into the skin and allows the removal of a cone of skin tissue), by shaving (a razor that removes a more superficial fragment of skin), by curettage, or by excision with a scalpel.
Chemical Cauterization – The application of a caustic or acidic substance over a lesion, with the objective of removing it. The most commonly used substances are trichloroacetic acid and potassium hydroxide. Several sessions may be necessary, depending on the type of lesion being treated.
Cryotherapy – Also known as cryosurgery, this is a therapeutic process based on the treatment of lesions by cold. Various chemical agents can be used in the abrupt cooling of the skin, liquid nitrogen being the most commonly used.
Curettage – A specific technique of scraping the lesion with a curette (a spoon-shaped, non-cutting surgical instrument). It can be done as a single procedure for superficial lesions or as part of more complex procedures such as electrodissection or cryotherapy.
Electrodissection or Electrocauterization – A procedure done with an electronic scalpel that destroys benign or malignant tumors through heat and electricity. Used to remove some types of benign tumors and some types of skin cancers.
Excision – Removal of the tumor with a scalpel, and also removal of an additional border of healthy skin as a safety margin. The removed tissue is examined under a microscope to see if all cancerous cells have been removed. It has high cure rates and can be used in the case of recurrent tumors.
Laser – Removal of the tumor cells using a carbon dioxide or erbium laser. Because it does not cause bleeding, it is an effective option for those with blood disorders.
Mohs Micrograph – Removal of the tumor and a fragment of surrounding skin with a curette. This material is then analyzed under a microscope. This procedure is repeated successively, until no traces of tumor cells remain. The technique preserves much of the healthy tissue and is indicated for cases of poorly delimited tumors or in critical areas.
Photodynamic Therapy (PDT) – A photosensitizing agent is applied (such as 5-ALA or 5-aminolevulinic acid) to the abnormal cells. After a period of time, the treated areas are exposed to an intense light that activates the 5-ALA and destroys the tumor cells, with minimal damage to healthy tissue.
BENIGN TUMORS (NON-CANCEROUS)
People should see a specialist if a spot, mole or wart itches, hurts, grows, has secretions or has not healed for a long time. Often, a skin tumor is more of a cosmetic problem. Few are cancerous, and the causes of most of them are unknown. Some are caused by viruses (like warts), systemic disease (like excess fat in the blood), genetics, and environmental factors (prolonged sun exposure).
The diagnosis of non-cancerous Skin Tumors and Lesions is made by physical examination and sometimes by pathology (biopsies). When they do not disappear on their own, planning for their respective treatments depends on characteristics such as location, type, and size. The most common types are:
Acrocordon or Soft Fibroma – This is a small, pedunculated, rounded, skin-colored or slightly darker soft elevation of 1 mm to 1 cm that usually appears on the neck, armpits, and groin. Common in obese people, diabetics, and in women. This annoying and unsightly lesion can be removed by cryotherapy, gentle electrodissection, or excision with a scalpel or scissors.
Ceratoacanthoma – Starts as a papular lesion on the epidermis that grows over 2 to 4 weeks to a size of 2 cm or more with a sunken (umbilicated), dark (keratinous) core. It appears in older people, more common in women, mainly on sun-exposed skin such as the forehead, nose, lower lip, hands, and arms. After 4 to 6 months, the nucleus may be expelled, leaving a whitish scar. It is almost always a benign tumor, but can be confused with a squamous cell carcinoma. In this case, it is removed by excision and may be sent for biopsy.
Actinic Keratosis – Also known as solar keratosis or senile keratosis (appears in older people), this is a skin condition characterized by a reddish, rough, flaking color. It is most common on the face, lips (actinic cheilitis), ear, back of the hand, forearm, scalp (in bald people), and neck. People with light skin, blond or red hair, and light eyes (blue or green) are most likely to have this tumor. As it can develop into squamous cell carcinoma, the indication is to be removed as a precaution by photodynamic therapy, cryotherapy, and curettage.
Seborrheic Keratosis – a superficial epithelial lesion 2 to 10 mm in diameter, with well-circumscribed rounded or irregular borders, brownish or brownish-black coloration, verrucous aspect, rough surface, but may occur as a smooth papule. It appears mainly on the face, trunk, fingers, and head. It can grow into a plaque several centimeters long. It usually has a genetic origin. It can be confused with melanoma, but it is an aesthetic problem and is asymptomatic. Removal is indicated only when it is irritated, pruritic or aesthetically uncomfortable. For this, we use cryotherapy or electrocoagulation associated with curettage.
Epidermoid Cyst – Formerly known as “sebaceous cyst” (a misnomer because it is not formed in the sebaceous gland), it is filled with keratin and lined by stratified squamous epithelium. It is triggered by a structural alteration in the follicle composition or when the cells that are in the most superficial layer of the skin (epidermis) end up going to the dermis, generating this cystic formation. It is round, mobile, has a fibroelastic consistency, the color of the skin itself, and can grow several centimeters. It usually appears on the back, face, and thorax of adults, and can be painful if it becomes infected. Surgical removal of the cyst (including its capsule) through an incision is indicated.
Cutaneous Horn – It is shaped like a conical horn, straight or curved, yellowish-white, can reach up to 13 cm, and originates from abnormal growth and keratinization of the skin. It is more common in old people, men, and whites. It can appear anywhere on the skin, including the lips. It can undergo malignant transformation. It can be removed by cryotherapy, electrodissection, or excision.
Dermatofibroma – Shaped like a firm papule or subcutaneous nodule, can have various colors such as brown, purple, red, yellow or pink, and grow to between 3 and 10 mm. The tumor can be caused by fibrous reactions to trauma, insect bite, viral infection, cyst rupture, or folliculitis, usually on the thigh and leg, but can occur anywhere. Most common in the immunosuppressed. Usually causes no symptoms. Diagnosis is made clinically and we recommend excision plus biopsy if problematic.
Pyogenic Granuloma – A scarlet-colored, fleshy, moist or crusted vascular nodule, usually composed of proliferated capillaries in a stroma. Diagnosis involves biopsy and histopathological examination. Occasionally, the lesion resembles a malignant tumor. Treatment consists of excision or electrodissection and curettage. The lesion may reappear.
Hemangioma – Also known as infantile hemangioma, this is a lesion that can be single or multiple and is located preferentially on the face, scalp and trunk. It is elevated, a few millimeters in size, rounded, shiny, and has a bright reddish color, similar to the color of a strawberry or raspberry. It affects more girls than boys (5:1 ratio), premature newborns, and low birth weight babies. It may disappear spontaneously without causing symptoms. It never becomes malignant. When medication does not resolve it and if there is significant cosmetic involvement, ulceration, and pain, it can be removed by excision or electrodissection and curettage.
Sebaceous Hyperplasia – This benign tumor that is between 2 and 5 mm in diameter develops when there is an increase in the size of the sebaceous gland due to androgenic hormones. It presents as a soft, yellowish, rounded papule, sometimes with a sunken center (umbilicated). More common in light-skinned adults and in people who have oily skin. More common on the forehead, cheeks, and nose with advancing age (hence also called “senile hyperplasia”). Diagnosed by clinical examination. A biopsy is indicated to rule out the possibility of a basal cell carcinoma. It can be removed by cryotherapy, electrodissection, peeling and laser.
Simplex and Malignant Lentigo – Both types are brown or brownish patches, smaller than 1.5 cm, circumscribed, with regular or non-regular borders, composed of localized proliferation of epidermal melanocytes. It can be hereditary or acquired. Its name refers to the appearance of the lentil. The simplex lentigo lesion is benign and appears in the first years of life on any part of the body or mucous membranes and multiplies with age, like freckles. The malignant lentigo lesion, despite its name, is pre-malignant, but can turn into a melanoma. It grows slowly over the years on areas frequently exposed to the sun, such as the face, neck, hands, and legs. It commonly appears in older people. It is the only variety of intraepidermal melanocytic dysplasia that is capable of developing into a melanoma in situ (without metastasis) and invasive (with metastasis).
Lipoma – A subcutaneous tumor composed of adipocytes (fat cells) that can be caused by genetic mutations or physical trauma. Commonly soft in consistency, round or oval elevation shape, most are painless and about 80% are less than 5 cm in diameter, but can reach more than 20 cm and weigh more than 1 kg. More common in women than men, it appears between the ages of 40 and 60. It tends to occur on the trunk, shoulders, neck, and armpits. It can move under the skin. If bothersome, it can be removed by excision or liposuction.
Nevus – Popularly known as a spot or mole, this congenital lesion has various sizes, can be flat or protruding, smooth or rough (warty), and can even have hair growing on it. It is not very high, red-brown or black in color, with well-defined borders. It is most common on the head, neck and trunk. It rarely grows into a melanoma, which it looks very similar to aesthetically. If a nevus is painful, itches, bleeds, or ulcerates, excisional biopsy may also be considered. If done, it does not increase the possibility of metastasis (if the lesion is malignant) and avoids extensive surgery on a benign lesion. If bothersome, it can be removed by excision or electrodissection.
Atypical Nevus – Also composed of nests of melanocytes, this type of lesion may have a higher risk of presenting melanoma. It has ill-defined, irregular borders and is dark to light brown in color. Constant close clinical monitoring and biopsy of that highly atypical or changing lesion is recommended in a patient with a high risk, personal or family history of melanoma. If indicated, removal is by excision or electrodissection and curettage.
MALIGNANT TUMORS (CANCEROUS)
Malignant Skin Tumors and Lesions correspond to about 30% of all cancers in Brazil, according to information from INCA (National Cancer Institute). The cutaneous ones are formed by cells that undergo genetic mutation and multiply in a disorganized way giving origin to a new tissue (neoplasm). They have the characteristic of spreading throughout the body (metastasis) and do not respect the limits of the surrounding normal skin.
Skin cancer mainly affects people with light skin, blonde or red hair, and light eyes who get sunburned easily and never tan (or tan with difficulty) or who have other dermatological disorders. About 90% of the lesions are located on the areas that are exposed to the sun. People over 40 are among the most affected population.
Besides the clinical examination, we use the biopsy to confirm the diagnosis. Among the treatments for malignant Skin Tumors and Lesions are excisional surgery, electrodissection with or without curettage, cryotherapy, photodynamic therapy, laser, radiation and topical medications. The most common are:
Basal Cell Carcinoma – Of the skin cancers, it is the least aggressive and the most frequent (70% of the diagnoses, according to INCA). It is an elevated, rounded, skin-colored or bright pink, painless, slow-growing lesion that invades tissue but rarely produces metastases. Most basal cell carcinomas arise from other tumors. Most common in sun-exposed places such as face and limbs. It is possible to remove all cancerous cells with surgery only, provided it is diagnosed in the early stages of development.
Squamous Cell Carcinoma – It is diagnosed in 25% of the cases of skin cancers in Brazil. This form of skin neoplasm arises in the squamous cells, which make up most of the upper layers of the skin (epidermis), and develops most in areas constantly exposed to the sun, such as the arms, legs, neck, face, and scalp. Long and excessive exposure to arsenic, tanning booths, X-rays, chronic infections, inflammation of the skin, and even spontaneous skin exposure can also give rise to squamous cell carcinoma. It spreads along the sides of the borders and new lesions usually appear near the old ones, and can evolve rapidly accompanied by secretion, itching, redness, scaling, cracking, and blood.
Melanoma – Although it represents less than 3% of skin cancers, it is the most aggressive type due to its high possibility of metastasis and high lethality. It can arise from melanocytes (skin pigment-producing cells whose major function is to help protect the body from the impacts of solar radiation) that grow rapidly, abnormally, and uncontrollably, and therefore can spread to other organs such as the lungs, brain, liver, bones, or intestines. One should be on the lookout for bleeding, itching, scaling, and pain in spots or moles all over the body. As we could not fail to mention, excessive exposure to sunlight is the main factor that can increase the risk of developing a melanoma. Timing is important in treatment. The earlier the diagnosis is made, the more superficial the disease is and with more chances of cure. Surgery is the most indicated treatment, however, radiotherapy and chemotherapy can also be used, depending on the stage of this malignant cancer.
There are other rare malignant Skin Tumors and Lesions such as Kaposi’s sarcoma (caused by the human herpes 8 virus in immunosuppressed people), Merkel cell carcinoma (touch cells), sebaceous carcinoma (sebaceous glands), seringoid carcinoma (glandular ducts), eccrine spiradenoma (sweat glands), among others.
The procedure must be performed in an office or hospital, according to the degree of complexity of the planned surgery. Likewise, the anesthesia can be local, with or without sedation, or even general, whatever is more comfortable and safer for the patient.
SKIN CANCER ABCDE
Always perform a self-exam for spots or moles on your skin and watch for characteristics that may indicate the presence of a malignant tumor, which can be:
ASYMMETRY – Is one half different from the other? The shape of the malignant tumor is unequal in its proportions.
BORDERS – They are wavy or ill-defined and irregular rather than rounded (or oval) and smooth.
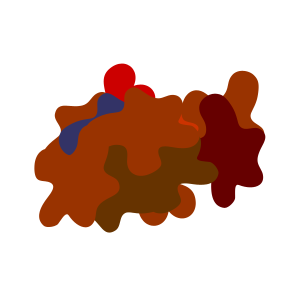
COLORS – Various shades from one area to another with black, brown and beige and different and unusual colors such as red, gray or bluish tones or light halos.
DIAMETER – In most cases the malignant lesion is larger than 6 millimeters.
EVOLUTION – It shows rapid growth or progressive modification in a short time to the sides and upwards.
TIPS ABOUT SUN EXPOSURE
Avoid prolonged sun exposure between 10 am and 4 pm – higher incidence of dangerous ultraviolet rays (UV) – protecting children and encouraging teenagers to protect themselves. Mainly the face region, lips and ears.
Use a good quality sunscreen daily, i.e. one that protects against UVA and UVB radiation and has a minimum of 30 SPF (sun protection factor). When you are at the beach or swimming pool, reapply it every 2 or 3 hours. Use appropriate sunscreen for the lips.
Look for shady places and protect yourself from the sun with clothes, caps or wide-brimmed hats, and sunglasses (preferably with UV protection). Prefer tents and sunshades made of cotton or canvas (absorb 50% of UV radiation) rather than nylon (absorb only 5% of UV radiation).
Regularly check your skin for suspicious spots or blemishes.
INDICATION
Whether for health or aesthetics, the malignant Skin Tumors and Lesions should be diagnosed and treated early, especially those that itch or hurt, are bothersome, do not heal and grow quickly. Even those of low lethality, which can cause mutilating or disfiguring lesions in exposed areas of the body, causing suffering and/or discomfort to the patients.
Not every skin lesion requires surgical removal. After the proper evaluation, we discuss with the patient the possible behaviors that vary from simple periodic follow-up, through non-surgical treatments, to the surgery itself.
When indicated, it is worth noting that each and every surgical procedure involves risks. Even when we perform the correct pre-operative evaluation, the best surgical planning, and all the post-operative care is taken, the benign or malignant tumor can reappear and a new surgical procedure or treatment may be required.
The choice of treatment is made based on the type, size, location and depth of the tumor, taking into consideration the patient’s age and general health conditions.
PREOPERATIVE
If the planning involves surgery in a hospital, it is very important to consult the SCHEDULED THE SURGERY? page which has a series of questions for us to talk about during consultations, to help you with your doubts, and where you will find recommendations for the day of the procedure.
Upon release, the patient receives all the necessary prescriptions and orientation regarding home care, medications, dressings, and the expected date of return for re-evaluation.
POSTOPERATIVE
Most procedures are done on an outpatient basis. Even in cases of surgery, the procedure rarely requires hospitalization. We prescribe medication if the pain and throbbing bothers you. Once you have stitches, we remove them between a week and 10 days.
The first 2 days should be of maximum rest, fundamental for healing. After surgery to remove any type of skin lesion, the operated site is sensitive, sore, reddish for a few days, depending on each person. Elimination of small volume of fluid from the wound or formation of crusts may occur.
The time it takes you to resume your normal routine depends on the extent, complexity and type of surgery you have undergone. Try to limit sudden and large movements. Avoid exercise and contact sports for at least three weeks.
Avoid as much as possible exposure of the scars to the sun for at least 3 months. Then, always with the use of sunscreen with a minimum of 30 SPF (sun protection factor).
We follow your case and pass on all the information and recommendations from medications, dressings, release to return to routine and even exercises.
